With Masks Set to Drop in New York and California Schools, a Pair of Studies Lay Out the Number of Cases That Could Trigger

Get stories like this delivered straight to your inbox. Sign up for The 74 Newsletter
Updated, Feb. 28
On Sunday, Gov. Kathy Hochul announced that New York state will end its mask requirement for schools and child care facilities starting Wednesday. “The day has come,” the governor said. On Monday, California Gov. Gavin Newsom said indoor masking will no longer be mandatory at schools and child care facilities after March 11. For students in Los Angeles Unified School District, masking appears to remain in place through the end of the year per an agreement between the district and the teachers union, although the timetable could be renegotiated. New York City Mayor Eric Adams already followed the governor’s lead, saying that he plans to drop the city’s school masking rule — along with vaccine requirements for restaurants, gyms and movie theaters — on March 7. Adams said his administration would continue to monitor COVID case rates and promised to make a final decision by Friday. “New Yorkers stepped up and helped us save lives by reaching unprecedented levels of vaccination,” he said in a statement.
In early February, a flurry of Democratic states including New Jersey, Massachusetts and Connecticut announced the end of their K-12 face-covering rules. Yet a few holdout states, and many individual districts, still require students to cover up without a set end date — and decision makers are seeking further clarity on when to safely drop the practice.
As if on cue, two new papers deliver a clear, quantitative look at just how many cases unmasking might trigger, helping school leaders set customized benchmarks for the end of mandates based on their community’s expressed goals.
“Instead of saying, ‘Well, you know, masks off, people get sick. Masks on, fewer people get sick,’ [officials can understand] what exactly the magnitude of these outcomes are,” said John Giardina, the lead author of one of the papers and a Harvard University Ph.D student.
His study, which was peer-reviewed and published Feb. 14 in JAMA Network, uses simulation modeling to identify the COVID transmission levels at which virus spread would stay in control even when classrooms are mask-optional.
It comes as New York Gov. Kathy Hochul said leaders in her state are considering metrics such as community COVID transmission levels and pediatric hospitalizations as they decide whether to lift the statewide school mask mandate in March. And California officials say they are examining student vaccination rates to announce on Feb. 28 when schools might be able to scrap their mask rules, even as health officials say the county will likely lift its indoor masking mandate for other settings by late March.
“We’re among the 13 states that have not ended their school masking requirements,” California Gov. Gavin Newsom said last week. “I have stated very clearly that on the 28th of this month we will be announcing a specific date. That date with destiny, the masks will come off, and we’ll do it in an appropriate manner.”
Meanwhile, the Centers for Disease Control and Prevention have signaled that they will be looking to update their face-covering guidance in the coming weeks, with an emphasis on preventing hospitalizations rather than avoiding transmission altogether.
The study Giardina published with co-authors from universities such as Stanford, Brown and Johns Hopkins allows decision makers to consider all of those metrics — case rates, vaccination levels and hospitalizations — simultaneously.
Using the ‘formula’
School leaders can select from three possible objectives: Avoiding all in-school transmission (which Giardina acknowledges may be an unrealistic standard), keeping the average additional cases due to unmasking below a specified level, such as 5 per month, or keeping the average additional hospitalizations under a threshold, such as 3 per 100,000 people per month.
Then, based on the share of students who have been inoculated with COVID vaccines, they can find the appropriate community transmission level for unmasking.

“If you have your goals and you have the context you’re in in your community when it comes to vaccination and how effective you think masks are, you could certainly look at that table as a kind of formula and say, ‘Should we take off masks, or shouldn’t we?’” Giardina told The 74.
He cautions, however, that the model used in the study relies on certain assumptions that decision makers should take into account. For example, it uses transmission rates from Delta rather than Omicron, and assumes a school with 638 students and 60 staff.
“I would still hope policymakers take all the uncertainties into account and how things might differ for each particular community,” he said.
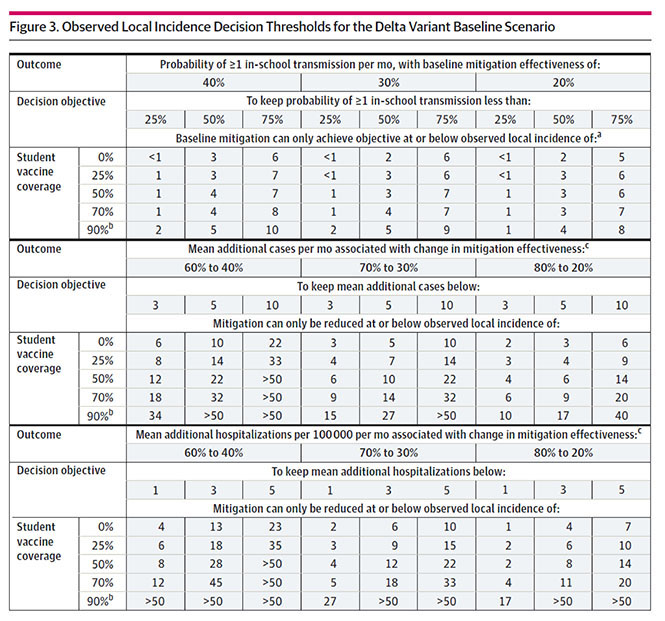
In the table above, schools can usually focus on the middle column, the researcher explained, which assumes the switch to mask-optional classrooms will decrease overall COVID mitigation effectiveness from 70 percent to 30 percent. But if the building has particularly effective ventilation, staving off some virus particles even when kids don’t cover up, they might push to the left column, where mitigation remains slightly higher even after scrapping face coverings. Conversely, if the school previously helped students access high-quality masks like KN95s, the dropoff in mitigation effectiveness when unmasking might be steeper, pushing schools to the right column.
A school with 50 percent student vaccination that assumes an average drop in protection without masks (middle column) and is willing to accept an average of up to 10 additional COVID cases per month due to the policy change could go mask optional once community transmission falls below 22 cases per 100,000 residents per day, according to the table. If the school increases its student vaccination rate to 70 percent, the threshold jumps to 32 cases per 100,000 because the stronger immunization rate will help stave off the higher community transmission rate.
Fifteen states and Washington, D.C. were at or below 22 cases per 100,000 residents per day, as of Feb 22. Another 15 were below 32 per 100,000. Nationally, case counts are trending downward, in some communities dramatically with 60 to 75 percent declines over the last 14 days.
Of the 500 largest U.S. school districts, 52 percent currently require students to wear masks, according to data collected by Burbio, which has tracked school policy through the pandemic. That’s down from 60 percent at the beginning of February, and other districts have mask-optional policies set to kick in in the coming weeks.
In New York, where no end to the statewide school masking rule has yet been specified, 58 percent of registered voters said they supported Gov. Hochul’s plan to review COVID data in early March before making any changes, while 30 percent thought the mandate should already have been lifted, according to a poll from the Siena College Research Institute released Tuesday. Another 10 percent said they wanted the policy to end after this week’s school vacation.
A second datapoint
As the move toward unmasking continues, a research brief out of Duke University’s ABC Science Collaborative corroborates Giardina’s findings, adding a second tool for school leaders to use in their decision making.
Like the study published in JAMA Network, the ABC Science Collaborative paper links school face-covering policies to additional likely COVID cases based on community transmission rates.
“You can see the differences in masking versus not masking and how many cases per week will happen in the community as a result of school policy,” said Danny Benjamin, professor of pediatrics at Duke and co-chair of the Collaborative, explaining his findings to educators in a Feb. 14 webinar. “You can then match these differences with your community’s risk tolerance as it relates to COVID.”
The paper, which the authors call a “blueprint” for navigating school policy this spring, draws on data from 61 school districts with varying mask rules. The researchers used those figures to then project the implications of mask-optional versus mask-required policies in a hypothetical 10,000-student school system.
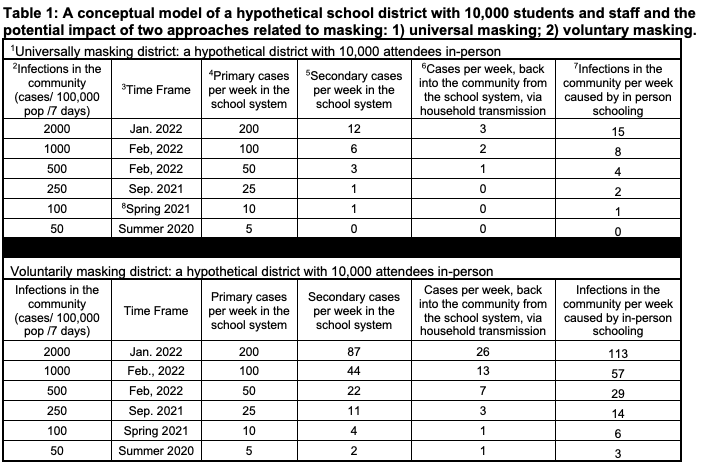
When community case rates are high, mask mandates prevent much would-be transmission, the authors found. In universally masked schools, it generally takes 20 to 25 COVID-positive individuals to set foot in the building for one case of in-school transmission to occur, said Benjamin, compared to other settings where the average infected person tends to pass the virus on to at least one other person.
“The short version is that masking clearly works,” he said.
However, when community case rates are low, the difference in prevented cases shrinks and school leaders may decide that enforcing a mandate is not worth the downsides. Research suggests that masks may hinder youngsters’ language and speech development and interfere with emotional recognition for people of all ages.
When case rates are just 100 per 100,000 residents per week, or about 14 per 100,000 per day (roughly the infection level before the Delta surge), districts with universal masking prevent only three additional cases compared to districts with voluntary masking. At 250 per 100,000 residents per week, where many communities currently stand, school mask mandates fend off an extra 10 cases in the district per week, the paper projects.
The brief does not break down expected cases by school vaccination rates. Nationwide, just under a quarter of children aged 5 to 11 and 56 percent of youth aged 12 to 17 are fully vaccinated against COVID-19, according to data from the American Academy of Pediatrics.
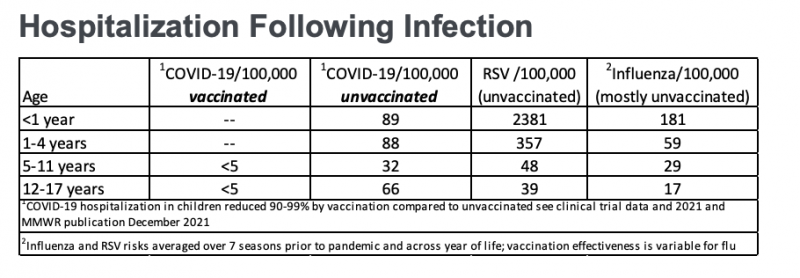
For some broader perspective, Benjamin reminded school leaders that children are just as likely or more likely to be hospitalized when they catch the flu or RSV compared to the coronavirus in all age groups except for 12- to 17-year-olds who have not been vaccinated against COVID.
Still, Benjamin’s co-chair at the Collaborative, Kanecia Zimmerman, emphasized that any shift in policy has implications not just for families’ physical health but also their mental health. An early February poll conducted by CBS News found that 57 percent of parents of school-aged children believe masks should still be required in school while only 36 percent said they should be optional. Another 7 percent want face coverings banned in classrooms.
Even when epidemiologically sound, a shift to voluntary masking may create distress for families, and the Duke associate professor of pediatrics urged school officials to consider bolstering the mental health supports available to students.
“Unmasking … is going to represent a substantial change for many families, for many districts, for many children,” she said. “When you’re making decisions about how to move forward, make those decisions in light of how you might be able to do things for the whole child.”
Get stories like these delivered straight to your inbox. Sign up for The 74 Newsletter

;)
